Osteology Case 10
Dr. Sharjeel Usmani
MBBS. MS. FRCP(E). KBNM. FANMB
Quiz
What is the diagnosis ?
a) Non-aggressive bone lesion at right parietal bone, likely enchondroma or fibrous dysplasia; for follow-up.
b) 18F-NaF uptake is likely in the calcified brain metastasis at parietal lobe of the brain. Advised MRI for confirmation.
c) Aggressive fusiform solitary osteoblastic bone lesion at right parietal bone is highly suspicious for bone secondaries; for further radiological evaluation.
d) 18F-NaF uptake is likely in the calcified meningeal lesion at parietal region of the brain is likely due to meningioma. Advised MRI for confirmation.
Scroll down for answer
Answer: d
d) Meningioma
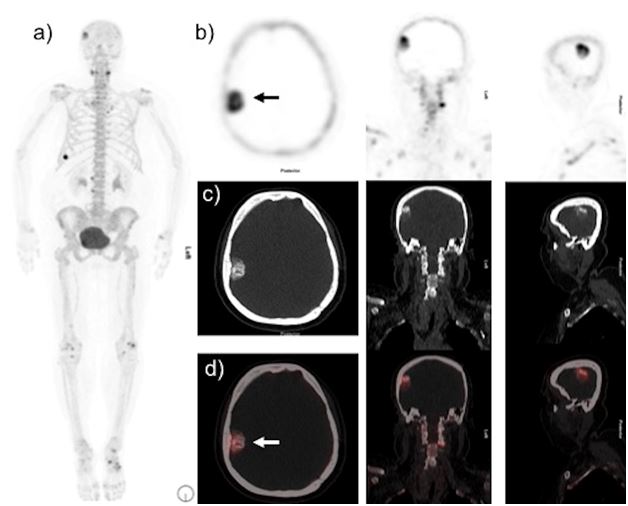
Non-contrast CT images showbroad-based calcified mass attached to the right parietal bonewith increased thickening of inner table of right parietal bone, massshowincrease tracer uptake on fused images. Meningioma was suspected. MRI and follow-up scan is advised.
Meningiomas are the most common duraltumourarise from the meningothelial cells of the arachnoid membranes, which are attached to the inner layer of the dura mater [1].It usually seen as an incidental finding on brain imaging and represent about 20% of all intracranial tumors. It is important to differentiate it from other mimics like primary neoplastic processes, metastases, granulomatous diseases and infection.
Meningiomas typically appear as lobular, extra-axial masses with a broad dural base. Typical features on unenhanced CT images are well-circumscribed, smoothly marginated extra-axial mass abutting the dura. Approximately 70-75% of meningiomas are hyperattenuating to surrounding brain parenchyma, while roughly 25% are isodense. Calcification is seen in approximately 20-25% of cases [2,3].
MRI is the modality of choice for evaluating meningiomas due to superior contrast and has ability to differentiate between intra- and extra-axial lesions. The typical MRI characteristically demonstrate, iso- to hypointensity on T1-weighted, and iso- to hyperintensity on T2-weighted images. Typically, meningiomas demonstrate homogeneous enhancement after contrast injection. however, the areas of central necrosis or calcification that do not enhance [4].
Meningiomas can be identified incidentally on bone scans likely because of calcification which thought to be seen in 25% of the meningiomas, other localization factors are presence/absence of a vascular pool [5]. Few case reports of 18F-NaF PET/CT also shows localization of 18F-NaF in meningiomas [6,7].Like conventional bone scintigraphy with 99mTc-MDP, 18F-NaF also accumulates in extra osseous lesions due calcification or calcifications within necrosis [8]. The mechanism of 18F-NaF uptake in calcified lesions is its direct incorporation into the hydroxyapatite crystal. 18F-NaF can accumulate in intracranial lesions due to both benign and malignant etiologies which include brain stroke, tumors, and metastatic lesions [9]. Clinical information and morphological information from correlative CT are essential for a correct diagnosis.
References:
- Weber DC, Lovblad KO, Rogers L. New pathology classification, imagery techniques and prospective trials for meningiomas: the future looks bright. CurrOpin Neurol. 2010;23:563–570.
- Morrison MC, Weiss KL, Moskos MM. CT and MR appearance of a primary intraosseous meningioma. J Comput Assist Tomogr. 1988; 12:169-70.
- Schubeus P, Schorner W, Rottacker C, et al. Intracranial meningiomas: how frequent are indicative findings in CT and MRI?. Neuroradiology. 1990; 32:467-73.
- Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics. 1991;11:1087–1106
- Rengachary SS, Batnitzky S, Arjunan K. Diagnosis of intracranial meningioma with radionuclide bone scan. Surg Neurol. 1980;14:337-41.
- Derlin T, Mester J, Klutmann S. Abnormal F-18 fluoride uptake in intracranial meningiomas on PET/CT. Clin Nucl Med. 2010;35:806–7
- Teo TY, Menda Y, McNeely P, et al. Incidental meningioma detected on 18F-fluoride with PET/CT during initial staging for prostate cancer. Clin Nucl Med. 2015;40:596–597.
- Usmani S, Gnanasegaran G, Marafi F, et al. The clinical significance of incidental soft tissue uptake on whole body 18F-Sodium Fluoride (NaF) Bone PET-CT: Pictorial Review. Clin Radiol. 2019;74:95-110.
- Wu J, Zhu H, Ji H. Unexpected detection of brain metastases by 18F-NaF PET/CT in a patient with lung cancer. Clin Nucl Med. 2013;38:e429–432.