Endocrinology case 3
11th September 2020
Endocrinology case 3
Case uploaded by Dr. Sharjeel Usmani
Kuwait
A 32-year-old female is a known case of papillary thyroid cancer. Treatment involved both thyroidectomy and ablation with I-131, three years back. Later on, follow-up revealed rising ATG titers.
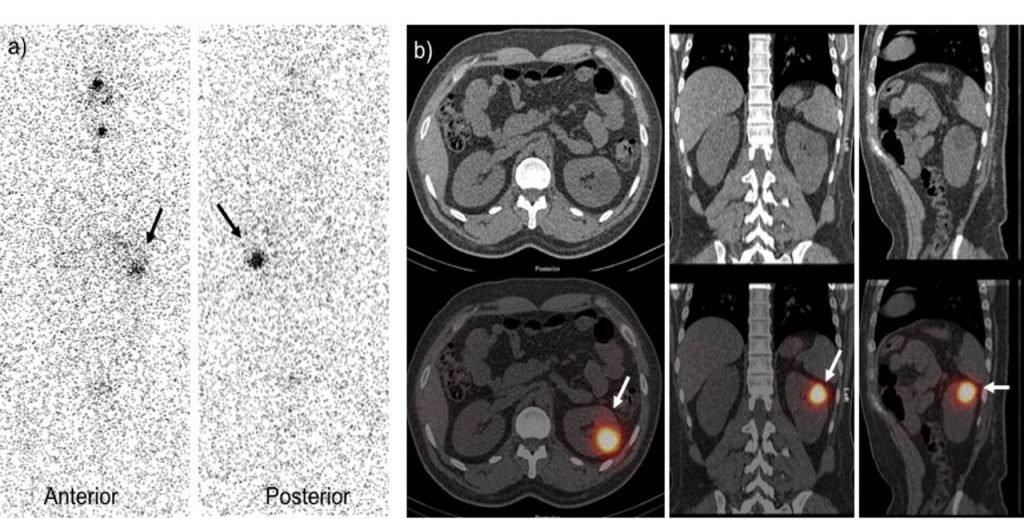
(a) The current study demonstrated I-131 uptake in the remnant thyroid tissue similar to the post ablation whole body scan. Focal increase tracer uptake is also seen at the left side of the abdomen (black arrow). SPECT-CT images (b) localize this uptake in the left kidney (white arrow). What is the diagnosis ?
- Physiologic radioiodine uptake in a simple cyst of the left kidney.
- Physiologic radioiodine uptake in the left pelvicalyceal system. Delayed images should be acquired.
- Uptake of radioiodine in the kidney is likely specific to thyroid metastases due to expression of sodium-iodide symporter (NIS) by tumor tissues.
- Uptake of radioiodine in complex cystic mass at left kidney according to bosniak classification further evaluation with contrast CT is required for better characterization.
Scroll down for answer and discussion
Answer:
- Physiologic radioiodine uptake in a simple cyst of the left kidney
Discussion
a) Whole body planar scintigraphy and b) SPECT/CT images demonstrate focal tracer uptake at the left side of the abdomen (arrows). SPECT/CT images revealed it as radioiodine uptake in a simple cyst of the left kidney. Communication between the cyst and the urinary tract, or secretion of radioiodine by the lining epithelium of the cyst can be causes of radioiodine uptake in the cystic structure.
Thyroid cancer is the most common type of endocrine-related cancer and representing 3.8% of all new cancer cases [[1]]. Differentiated thyroid cancer (DTC), which includes papillary and follicular cancer, comprises the vast majority (>90%) of all thyroid cancers [[2]]. Radioiodine is been used for diagnosis and treatment of patients with DTC. The enhanced expression of sodium-iodide symporter (NIS) is a key mechanism of radioiodine uptake in functioning thyroid tissues [[3]]. The uptake of radioiodine in thyroid metastases also depends on expression of NIS by tumor tissues. However, because radioiodine may also accumulate in normal structures and tissues, it is important to distinguish physiologic radioiodine activity from metastatic disease. SPECT/CT scans may accurately localize and help differentiate benign mimics of disease, with the potential to alter the management plan. It has emerged as a powerful tool for assessing unexpected concentrations of radioiodine resulting from benign uptake in organs with NIS expression, radioactive secretions or excretory products, inflammation, or other mechanisms of uptake [[4]].
Various cystic structures, including the nasolacrimal sac, pleuropericardial, bronchogenic, thymic, breast, hepatic, renal, ovarian, epithelial and sebaceous cysts are also known to show false-positive findings on radioiodine WBS [[5]]. False positive radioiodine uptake in the renal cysts has been reported in literature [[6],[7]]. There are various hypotheses of the pathophysiology behind uptake in renal cysts including an active secretory process by the renal tubules and communication between the cyst and the renal collecting system [[8]]. Another author suggested that the entry of radioiodine into cysts occurs via passive diffusion or partially active transport; then, due to the slow exchange of water and chemical elements between the cysts and their surrounding extracellular/extravascular environment, it becomes trapped within the cysts [[9]].
References:
[1]. National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER). SEER Stat Fact Sheets: Thyroid Cancer. http://seer.cancer.gov/statfacts/html/thyro.html. Accessed December 21, 2016
[2]. Enewold L, Zhu K, Ron E, et al. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiol Biomarkers. 2009; 18: 784–791
[3]. Chung JK. Sodium iodide symporter: its role in nuclear medicine. J Nucl Med. 2002;43:1188–1200.
[4]. Wong KK, Zarzhevsky N, Cahill JM, et al. Hybrid SPECT-CT and PET-CT imaging of differentiated thyroid carcinoma. Br J Radiol. 2009;82:860–876.
[5]. Bural GG, Peel RL, Mountz JM. Benign epithelial cyst mimicking thyroid cancer metastasis: a false-positive finding on post-therapy I-131 scan. Clin Nucl Med. 2012;37:88–90
[6]. Wen C, Iuanow E, Oates E, et al. Post-therapy iodine-131 localization in unsuspected large renal cyst: possible mechanisms. J Nucl Med. 1998;39:2158–61.
[7]. Letaief B, Boughattas S, Guezguez M, et al. Abdominal uptake of I-131 revealing a renal cyst. Clin Nucl Med. 2001;26:255–6.
[8]. Campennì A, Ruggeri RM, Giovinazzo S, et al. Radioiodine uptake in a renal cyst mimicking a metastasis in a patient affected by differentiated thyroid cancer: case report and review of the literature. Annals of Nuclear Medicine. 2014;28:472–476.
[9]. Oh J-R, Ahn B-C. False-positive uptake on radioiodine whole-body scintigraphy: physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging. 2012;2:362–385.